Polio shows us the way for COVID (repost from Twitter)
From time to time, I’ll be reposting content from Twitter here so I have it for posterity.
This is probably my most popular thread on COVID,1 posted 22 July 2022 and mirrored on Typefully, in which I talk through the history of polio and what it tells us about how santitation and vaccination can interact to eliminate a highly infectious pathogen. I’m not terribly optimistic about mucosal vaccines for SARS-2, but the overall arguments stand, and I’ll take thrice yearly boosters with humoral vaccines as a similarly effective consolation prize if I can!
The thread has been lightly modified for this format.
MFW all the hot takes on SARS2, polio, transmission blocking, mucosal immunity, and community-level risk differences collide! 🤯
The story of polio epi today is the story of how mucosal vaccines and clean indoor air will together be transformative against respiratory infections.
The ability of polio to transmit depends most strongly on contact network density, water and sewer sanitation, and immunity against infection (both mucosal and systemic). I will thread all these together below and point the way toward a much better future for SARS2, flu, etc.
Contact network density has the same effects on polio as for any communicable disease. More contacts = more transmission. But because the transmission routes are fecal-oral and oral-oral, it’s mostly intimate friend and family contacts that matter except where sanitation is poor.
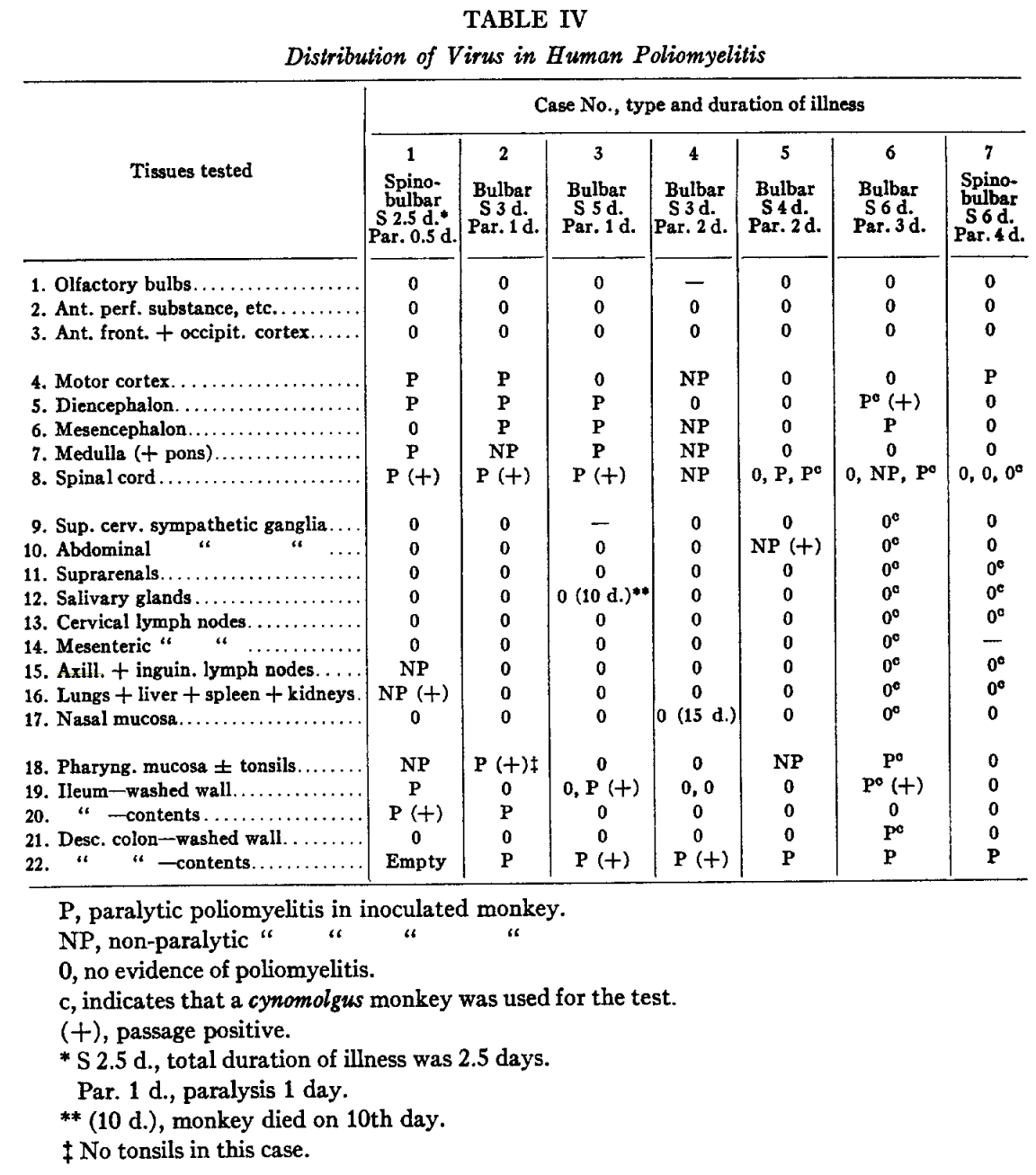
(As an aside, respiratory transmission was debated heavily back in the day, but was determined insignificant because poliovirus is only rarely found in lungs and nasal mucosa. The dismissal of the airborne route is grounded in biology and not sloppy epi. An early reference from Sabin showing where poliovirus is found upon autopsy provides the table below.)
So, poliovirus transmission rates depend on social context, but transient superspreading through indoor air is unlikely to be a big factor. Rather, the first big factor is water and sewer sanitation.
The story of polio and sanitation is rich and fascinating. If you read one article, choose this: From Emergence to Eradication: The Epidemiology of Poliomyelitis Deconstructed.
In towns and cities without closed sewer and water systems, polio is at least as infectious as measles. Historically, almost everyone got the multiple strains very young, when protected from paralysis by maternal antibodies, and so “infantile paralysis” was sporadic and rare. As sanitation improved throughout the late 19th and 20th centuries in much of the world, polio became an epidemic disease because people started getting it when they were older and no longer had maternally-acquired protection. Vaccination interrupts this in ways discussed below.
But, as sanitation improves even further, to reach standards most who live in high and middle income countries take for granted today, sanitation interacts with vaccination to become a friend again. (Immodestly) if you read one, choose Assessing the stability of polio eradication after the withdrawal of oral polio vaccine.
Sanitation determines the typical fecal-oral exposure–how much poop you eat–under different living conditions. Everyone eats some poop everyday, but we infer that typical amounts vary by at least 4 orders of magnitude. So in some places, polio transmits through food, dirty water, latrines, touches, all sorts of different surfaces and fomites, (maybe flies) and… In other places, it only likely transmits via direct contact with oral secretions or something that has been in someone’s mouth.
This brings us to the role of vaccination and infection-blocking immunity. Why? Polio immunity is multifaceted and the effectiveness of vaccination against transmission depends strongly on sanitation! There are two immunologically-relevant “compartments”. Enteric mucosal immunity that prevents infections in the gut (primary site of polio infection) and systemic humoral immunity that prevents proliferation of poliovirus from the gut to other parts of the body.
IPV, the Salk vaccine, when given to someone who’s never had a live poliovirus infection, provokes excellent humoral immunity but almost-zero enteric immunity. So IPV rocks against paralysis (can’t get to neurons) AND oral shedding, but not infection or fecal shedding. So if you live somewhere with reliable water and sewer sanitation and where hand, food, and toilet hygiene standards are high, IPV alone will prevent both paralysis and transmission. This applies to most people in high and middle income countries. But, IPV alone doesn’t do anything to prevent infection in the gut, and so it does nothing to prevent fecal-oral transmission. Thus, people who live in places without effective sewage and water sanitation infrastructure, or less hygienic practices, polio will still transmit.
Here enters OPV, the Sabin vaccine. OPV is a live-attenuated vaccine that is very similar to a wild poliovirus except it is 1-10 thousand times less likely to cause paralysis (depending on the strain). This replicates in the gut and provokes strong mucosal and humoral immunity. So OPV vaccination can shut down transmission in places without good sanitation. Hence its use in eradication, both historically in countries like the US that can now maintain elimination with IPV alone but couldn’t do so 60 years ago, and in places where polio remains today.
(Another aside: the catches with OPV are it doesn’t cause zero paralysis and it’s not different enough from wild poliovirus when it comes to transmission. That’s also a fascinating and difficult story, worked through in detail here (again), but not this thread’s story.)
In summary, the epi of polio today is one where it does or can transmit only in communities that have the wrong combinations of under-vaccinated, insufficient vaccine effectiveness for their sanitary conditions and contact networks, and/or insufficient sanitation and hygiene.
Back to the top, I wanna highlight two lessons of polio for SARS2, flu, etc. The effectiveness of infection-blocking immunity depends on exposure. Large changes in exposure can lead to different transmission dynamics. Together, the epi can change drastically.
First, effective mucosal vaccines, if we can get ones that work in humans, will be great for reducing transmission. I feel like an optimistic but maybe realistic dream would be 80% effectiveness against infection that lasts for a year against all known circulating variants. 80% effectiveness turns R0=10 into Re=2, which would probably lead to SARS2 settling down into an influenza-like annual incidence. That sucks less than not having mucosal vaccines, but with long COVID at appreciable rates across all ages, it still sucks.
Similarly, as shown by Josh Schiffer and colleagues (and others) and excerpted below, there is a dose-response relationship to SARS2 transmission. With realistic indoor air interventions using current technology, we can pretty easily imagine reducing viral loads in the air also by a factor of 5 or so in lots of spaces.
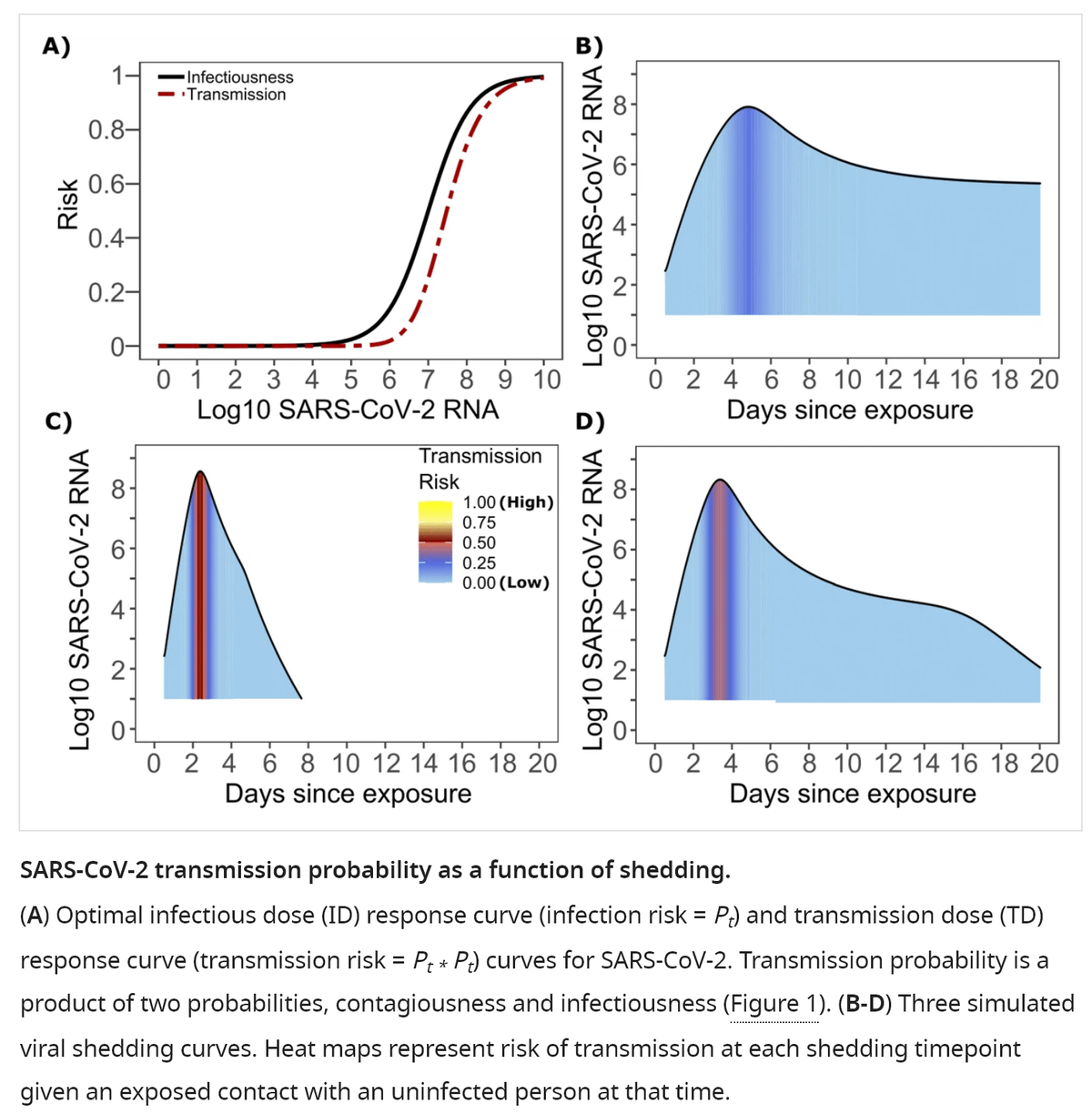
Realistic indoor air interventions applied at scale would turn R0=10ish to Re=2ish, which is much better than where we are today (for ex, it would eliminate flu and rsv – much better than vaccines alone), but still kinda sucks, because long COVID and an IFR still worse than flu.
I mean sure, these both look a lot more like influenza (but lurking long covid) and everyone this entire pandemic has framed a good outcome with SARS2 to be turning it into influenza, so that’s pretty good right? But imagine combining mucosal vaccines and clean indoor air!
Combine 5x reduction in airborne viral load with a 5x reduction from mucosal vaccines and R0=10ish turns into Re=0.4ish. That’s a pathogen that only circulates when either vaccination isn’t happening or your clean air infrastructure fails. JUST LIKE WHAT HAPPENED TO POLIO.
Clean air and mucosal vaccines working together is also more tolerant to the transient failure of either one. Say a new variant pops up and infection-blocking immunity goes to zero. We still have Re=2ish and very low prevalence. That gives more time to update vaccines. Better. Or say mucosal vaccines don’t work. We get infection-blocking from today’s vaccines, but transient and variant-dependent. But w/ Re=2 from clean air, less vax efficacy is needed. With help from seasonality, both could annualize epidemics and make booster timing feasible. Better. Or take spaces where we can’t achieve a 5x cut in airborne virus. Those still have reduced R0. Many crowds cease to be superspreading environments. Restaurants and homes can be crowded with similar risks to flu, and transmission is still stopped in the clean air places. Better.
This is also the story of polio. Once you break the global transmission network, susceptible pockets can go years without infections. With the network broken, infrastructure and vaccination programs can wobble without massive epidemics. Just like with polio.
And as with polio, there will still be endemic reservoirs wherever we can’t achieve the right combo of vaccine effectiveness and sanitation to bring R0 below 1. We will still have the problem of SARS2 anywhere is a threat everywhere–the fundamental challenge of global health. But that’s much better than the near future we’re facing today. Indoor air quality infrastructure is essential, and mucosal vaccines will make a big difference, but the two combined will be transformative!
We’re not used to thinking about this because we’re not used to thinking about how vaccine effectiveness and environmental conditions interact. The polio literature is messier than the story I told because the synthesis that ties it all together is spread over a 150 years. We’re not used to thinking about the setting-dependence of respiratory vaccines because, without mechanical indoor air cleaning, the range of variation in sanitation across human societies is more like a factor of 10 than the factor of 10,000 or more for sewage and water.
But we should be thinking about sanitation and vaccines together.
Vax and sanitation together tells you why it’s very unlikely that polio will explode in most of the world it’s been absent from for years. Just as it explains why it’s so hard to eradicate in places it persists, and why outbreaks happen where they do. Vax and sanitation together tells you why some of us still imagine a world where endemic circulation of respiratory pathogens has gone the way of polio, and that it can be achieved with incremental improvements in existing tech, without “lockdowns” or masking forever.
But we have to stop being so damned insular and start learning from each other! And learning from the past. I hope maybe the afternoon spent writing this helps someone out there.
For attribution, please cite this work as
Famulare (2023, June 20). Polio shows us the way for COVID (repost). Retrieved from https://famulare.github.io/2023/06/20/Polio-shows-us-the-way-for-COVID-repost.html
-
Second-most-popular it turns out. Helping people understand the sitation headed into Thanksgiving 2020 was #1. I suppose I feel good about that–I’m sure that thread saved lives. But I don’t know how well we learned its lessons. Maybe this one will do more over time. One can dream anyway. ↩